Services in our Office
Our goal is to provide exceptional care from diagnosis to treatment. Henein Arthritis and & Osteoporosis Center P.C. uses cutting-edge technology to complement our highly trained doctor and staff. Some of the on-site resources immediately available include:
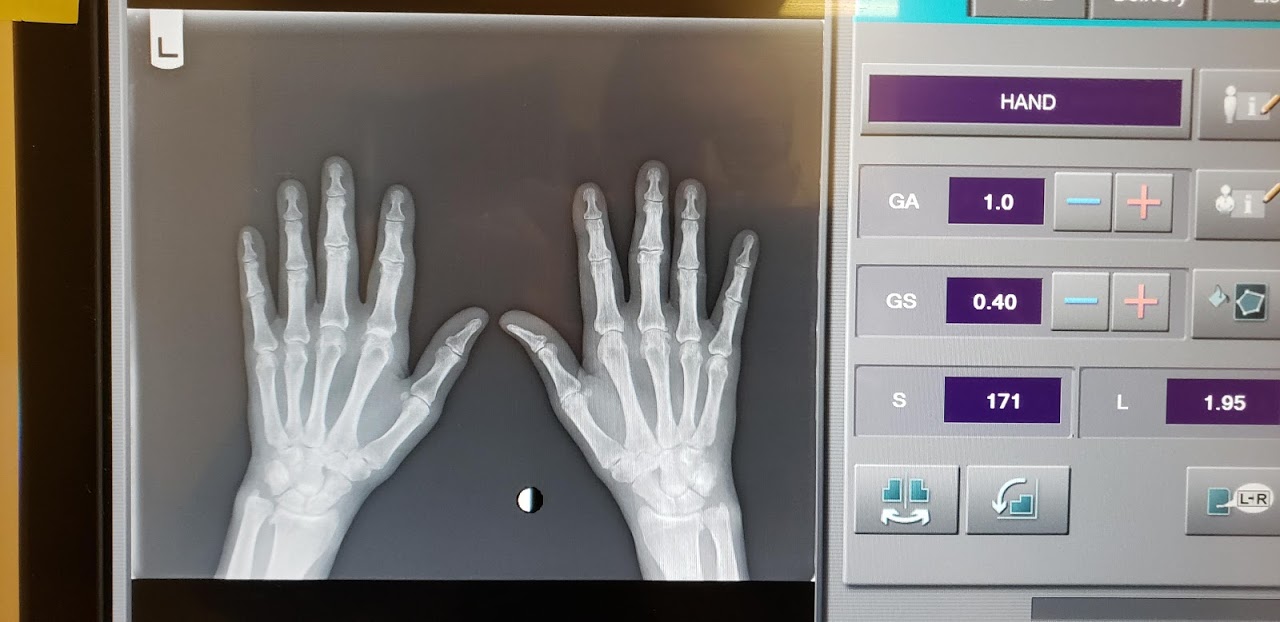
- Digital X-Rays
- Bone Density
- Phlebotomy
- Musculoskeletal Ultrasound
Our Services
Conditions that we treat at Henein Arthritis and & Osteoporosis Center, P.C.
At Henein Arthritis and & Osteoporosis Center, P.C., our philosophy is that each patient is on a journey to getting back to doing more of the things that they love. Our goal is to help you manage your condition in a way that allows you to live your life to the fullest.
Note: Click on any disease below to get more information about it.
Arthritis
What is arthritis?
Arthritis, or more specifically osteoarthritis, is a painful condition that develops when joint surfaces begin to degrade and break down, leaving bare bone ends exposed and resulting in inflammation, stiffness and loss of mobility in the joint. While arthritis can affect any joint, it occurs most commonly in the knees, hips, spine and neck, ankles, wrists and hands. Arthritis can affect anyone at any age, but it is much more common as we age. Another type of arthritis, rheumatoid arthritis, is an autoimmune condition that occurs when the immune system attacks healthy joint tissue.
What causes arthritis to develop?
Arthritis can develop as a result of traumatic injury or disease that affects the joints, and it can also occur following surgery. Most osteoarthritis develops in people as they age and years of wear and tear break down the joint surfaces.
What are the symptoms of arthritis?
Osteoarthritis causes symptoms like pain and swelling in the joints, warmth and tenderness in the area above joints, decreased range of motion, and stiffness, especially after a period of inactivity. Symptoms can range from mild to severe, and if left untreated, they can eventually have a serious impact on your quality of life.
How is arthritis treated?
Arthritis treatment begins with a thorough evaluation to determine your specific symptoms and the extent of the disease. Medications can help decrease pain and inflammation, and physical therapy, aquatics and therapeutic exercise can help keep joints flexible and restore mobility. Lifestyle changes like losing weight can also help by decreasing added strain on the joints, and assistive devices like canes and walkers can help you stay mobile and also decrease strain and discomfort. In more severe cases, corticosteroid joint injections can help relieve inflammation at the source. If joint surfaces are badly affected, joint replacement surgery may be considered.
Rheumatoid Arthritis
What is rheumatoid arthritis?
Rheumatoid arthritis is an autoimmune disease that causes the immune system to attack the healthy tissues of the joints, causing them to become painful and inflamed. Over time, chronic inflammation can destroy the joint tissues and cause joints to become deformed, limiting your ability to perform regular activities, including walking and using your hands. More common among women than men, rheumatoid arthritis typically begins between ages 40 and 60.
What causes rheumatoid arthritis?
The underlying cause of rheumatoid arthritis is not known, but researchers do feel genetics plays a role. However, studies have shown rheumatoid arthritis is not hereditary, which means having a family member with the disease does not make it more likely you’ll develop it yourself, nor can you pass it down to your children. Researchers believe the disease process is triggered when a bacterium, virus or other foreign “invader” causes the immune system to malfunction.
What are the symptoms of rheumatoid arthritis?
Joint pain and swelling are the primary symptoms of rheumatoid arthritis and can develop over a period of months. Joint stiffness and persistent fatigue often occur even before pain and swelling are observed. Low-grade fever, weight loss, loss of appetite and formation of nodules or lumps over pressure points are also common symptoms in people with rheumatoid arthritis. Rheumatoid arthritis typically occurs symmetrically, affecting the same joint on both sides of the body – for instance, both elbows or both knees. Joints in the hands, wrists, ankles, feet and neck are also commonly affected. Stiffness often occurs after prolonged periods of resting and may persist for several hours.
How is rheumatoid arthritis treated?
To some degree, treatment can vary based on your symptoms and how far the disease has progressed. Medicines, exercise or physical therapy, and lifestyle changes are usually all part of any treatment regimen. There is no cure, and treatment is ongoing.
Osteoarthritis
Osteoarthritis is the most common form of arthritis, affecting millions of people worldwide. It occurs when the protective cartilage that cushions the ends of your bones wears down over time.
Although osteoarthritis can damage any joint, the disorder most commonly affects joints in your hands, knees, hips and spine.
Osteoarthritis symptoms can usually be managed, although the damage to joints can’t be reversed. Staying active, maintaining a healthy weight and some treatments might slow progression of the disease and help improve pain and joint function.
Risk factors
Factors that can increase your risk of osteoarthritis include:
- Older age. The risk of osteoarthritis increases with age.
- Sex. Women are more likely to develop osteoarthritis, though it isn’t clear why.
- Obesity. Carrying extra body weight contributes to osteoarthritis in several ways, and the more you weigh, the greater your risk. Increased weight adds stress to weight-bearing joints, such as your hips and knees. Also, fat tissue produces proteins that can cause harmful inflammation in and around your joints.
- Joint injuries. Injuries, such as those that occur when playing sports or from an accident, can increase the risk of osteoarthritis. Even injuries that occurred many years ago and seemingly healed can increase your risk of osteoarthritis.
- Repeated stress on the joint. If your job or a sport you play places repetitive stress on a joint, that joint might eventually develop osteoarthritis.
- Genetics. Some people inherit a tendency to develop osteoarthritis.
- Bone deformities. Some people are born with malformed joints or defective cartilage.
- Certain metabolic diseases. These include diabetes and a condition in which your body has too much iron (hemochromatosis).
Treatment
Osteoarthritis can’t be reversed, but treatments can reduce pain and help you move better.
Medications
Medications that can help relieve osteoarthritis symptoms, primarily pain, include:
- Acetaminophen. Acetaminophen (Tylenol, others) has been shown to help some people with osteoarthritis who have mild to moderate pain. Taking more than the recommended dose of acetaminophen can cause liver damage.
-
Nonsteroidal anti-inflammatory drugs (NSAIDs). Over-the-counter NSAIDs, such as ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve, others), taken at the recommended doses, typically relieve osteoarthritis pain. Stronger NSAIDs are available by prescription.
NSAIDs can cause stomach upset, cardiovascular problems, bleeding problems, and liver and kidney damage. NSAIDs as gels, applied to the skin over the affected joint, have fewer side effects and may relieve pain just as well.
- Duloxetine (Cymbalta). Normally used as an antidepressant, this medication is also approved to treat chronic pain, including osteoarthritis pain.
Therapy
- Physical therapy. A physical therapist can show you exercises to strengthen the muscles around your joint, increase your flexibility and reduce pain. Regular gentle exercise that you do on your own, such as swimming or walking, can be equally effective.
- Occupational therapy. An occupational therapist can help you discover ways to do everyday tasks without putting extra stress on your already painful joint. For instance, a toothbrush with a large grip could make brushing your teeth easier if you have osteoarthritis in your hands. A bench in your shower could help relieve the pain of standing if you have knee osteoarthritis.
Surgical and other procedures
If conservative treatments don’t help, you may want to consider procedures such as:
- Cortisone injections. Injections of corticosteroid medications may relieve pain in your joint. During this procedure your doctor numbs the area around your joint, then places a needle into the space within your joint and injects medication. The number of cortisone injections you can receive each year is generally limited to three or four injections, because the medication can worsen joint damage over time.
- Lubrication injections. Injections of hyaluronic acid may offer pain relief by providing some cushioning in your knee, though some research suggests these injections offer no more relief than a placebo. Hyaluronic acid is similar to a component normally found in your joint fluid.
- Realigning bones. If osteoarthritis has damaged one side of your knee more than the other, an osteotomy might be helpful. In a knee osteotomy, a surgeon cuts across the bone either above or below the knee, and then removes or adds a wedge of bone. This shifts your body weight away from the worn-out part of your knee.
- Joint replacement. In joint replacement surgery (arthroplasty), your surgeon removes your damaged joint surfaces and replaces them with plastic and metal parts. Surgical risks include infections and blood clots. Artificial joints can wear out or come loose and may need to eventually be replaced.
Fibromyalgia
What is fibromyalgia?
Fibromyalgia is a painful and chronic disorder that affects about 5 million people in the U.S., causing widespread discomfort and tenderness, among other symptoms. Although some of the symptoms may feel like arthritis, fibromyalgia does not cause the joint damage associated with arthritis. However, it can significantly affect a person’s quality of life and their ability to carry on normal activities of daily living. About 80 percent to 90 percent of cases affect women, with men and children comprising the remaining cases.
What causes fibromyalgia?
The cause of fibromyalgia is not known, but research suggests chronic stress and traumatic injury, such as a car accident, may precipitate its development. Repetitive stress injuries and illnesses may also trigger fibromylagia. Many researchers have suggested genetic causes or problems with the way the central nervous system interprets and responds to pain signals.
What are the symptoms of fibromyalgia?
In addition to widespread and chronic pain, patients with fibromyalgia typically experience other symptoms, such as:
- chronic fatigue
- cognitive issues, including memory problems and difficulty concentrating (so-called “fibro fog)
- problems sleeping
- persistent headaches
- numbness in fingers or toes
- irritable bowel syndrome
- painful menstruation
- morning stiffness
- increased sensitivity to temperature extremes
- restless leg syndrome
- heightened sensitivity to bright lights and loud noises
Many patients have other chronic pain syndromes in addition to fibromyalgia, including temporomandibular joint disorder (TMJ), inflammatory bowel disease or interstitial cystitis.
How is fibromyalgia treated?
There is no cure for fibromyalgia, but several medications are being used to help relieve symptoms, including medications used both to treat depression and to treat chronic pain caused by damage to the central nervous system. Individual symptoms may also be alleviated with medications to reduce pain and inflammation. For some patients, physical therapy may provide some relief.
Gout
What is gout?
Gout is a condition that causes pain and inflammation in the joints. It occurs when sharp crystals of uric acid build up in the blood and are deposited in soft tissues, including the tissues of the joints. Uric acid is a naturally-occurring substance that’s usually eliminated through urine. But sometimes, uric acid can’t be efficiently eliminated, leaving it to build up in the soft tissues where it causes painful symptoms. Gout attacks are often preceded by chronic stress, illness or alcohol or drug use.
What are the symptoms of gout?
Gout occurs in four stages. In the first stage, uric acid levels are elevated in the blood, but there are no noticeable symptoms. In the second stage, joint pain and swelling develop, often very quickly. Most commonly, joint symptoms occur in the big toe or elsewhere in the foot or ankle, but they may also occur in the knees, wrists, fingers and elbows. Kidney stones may also develop. In the third stage, gout symptoms may subside and you may experience a decrease in pain and inflammation. The fourth stage is called chronic tophaceous gout, and this is the time when gout causes permanent damage to the joints and often, the kidneys.
What are the risk factors for gout?
Gout occurs more commonly in people who:
- are obese or overweight
- have a family history of gout
- consume a diet high in purines (the precursor of uric acid) or drink too much alcohol
- take certain types of medications, including diuretics
- have health problems like high blood pressure, diabetes, thyroid disease, renal insufficiency or psoriasis
How is gout treated?
In most cases, gout can be treated very successfully with non-steroidal anti-inflammatory drugs (NSAIDs) or corticosteroids to help relieve pain and inflammation. Dietary and lifestyle changes may also help reduce the amount of uric acid that’s produced.
Psoriatic Arthritis
Psoriatic arthritis is a form of arthritis that affects some people who have psoriasis — a condition that features red patches of skin topped with silvery scales. Most people develop psoriasis first and are later diagnosed with psoriatic arthritis, but the joint problems can sometimes begin before skin patches appear.
Joint pain, stiffness and swelling are the main signs and symptoms of psoriatic arthritis. They can affect any part of your body, including your fingertips and spine, and can range from relatively mild to severe. In both psoriasis and psoriatic arthritis, disease flares may alternate with periods of remission.
No cure for psoriatic arthritis exists, so the focus is on controlling symptoms and preventing damage to your joints. Without treatment, psoriatic arthritis may be disabling.
Both psoriatic arthritis and psoriasis are chronic diseases that get worse over time, but you may have periods when your symptoms improve or go into remission alternating with times when symptoms become worse.
Psoriatic arthritis can affect joints on just one side or on both sides of your body. The signs and symptoms of psoriatic arthritis often resemble those of rheumatoid arthritis. Both diseases cause joints to become painful, swollen and warm to the touch.
However, psoriatic arthritis is more likely to also cause:
- Swollen fingers and toes. Psoriatic arthritis can cause a painful, sausage-like swelling of your fingers and toes. You may also develop swelling and deformities in your hands and feet before having significant joint symptoms.
- Foot pain. Psoriatic arthritis can also cause pain at the points where tendons and ligaments attach to your bones — especially at the back of your heel (Achilles tendinitis) or in the sole of your foot (plantar fasciitis).
- Lower back pain. Some people develop a condition called spondylitis as a result of psoriatic arthritis. Spondylitis mainly causes inflammation of the joints between the vertebrae of your spine and in the joints between your spine and pelvis (sacroiliitis).
Lupus
What is lupus?
Lupus is a chronic autoimmune condition that develops when the immune system malfunctions and begins to recognize healthy cells and tissues as “foreign invaders.” In response, the immune system triggers a chemical reaction, releasing antibodies that begin attacking these healthy tissues and destroying them. While some autoimmune diseases attack one type of tissue or organs, in lupus the attacks are widespread and may involve the joints, skin, lungs, heart, kidneys and brain.
What causes lupus?
The cause of lupus is unknown, but research shows the disease is more likely to occur in people with relatives who also have it, suggesting a genetic component. Lupus symptoms can also be triggered by stress, disease, certain medications – even exposure to sunlight.
What symptoms does lupus cause?
Lupus can cause an array of symptoms, but very few people experience all of them. The most common symptoms include:
- rash, often on the cheeks and nose
- inflamed, painful joints
- swollen glands
- unexplained fever
- memory problems or difficulty focusing
- extreme fatigue
- sun sensitivity
- unusual loss of hair
- circulation issues causing pale or purplish toes or fingers and coolness
- seizures
- mouth sores
- kidney dysfunction
- multiple miscarriages
How is lupus diagnosed?
Lupus can be difficult to diagnose, partly because it doesn’t always cause severe symptoms, and partly because the symptoms it does cause can also be caused by other diseases and disorders. Providing a detailed medical history and a description of all your symptoms is the best way to help your healthcare provider arrive at the proper diagnosis. Lab tests can also help rule out other possible causes.
How is lupus treated?
Treatment depends on the symptoms you’re experiencing. Anti-inflammatory medications may be prescribed, as well topical creams for rashes. Corticosteroids, anti-malarial drugs and monoclonal antibodies are also commonly prescribed. Your treatment will be customized specifically for your symptoms.
Autoimmune Disease
What is an autoimmune disease?
Autoimmune diseases occur when the immune system malfunctions, causing immune cells called antibodies to mistakenly attack healthy tissue. More than 80 autoimmune diseases exist, affecting millions of men, women and children in the U.S. In most cases, researchers are unclear what causes the immune system to attack healthy tissues, but they do know the malfunction can often be triggered by illness, trauma, chronic stress, environmental pollutants or other factors.
What types of autoimmune diseases are there?
There are literally dozens of autoimmune diseases on record. Some of the most prevalent include:
- rheumatoid arthritis
- multiple sclerosis
- type I diabetes
- psoriasis
- Graves’ disease
- Sjogren’s syndrome
- lupus
- Hashimoto’s thyroiditis
- celiac disease
- Addison’s disease
What symptoms do autoimmune diseases cause?
Autoimmune diseases can cause a wide array of symptoms, depending on the type of disease that’s present. Some common symptoms include:
- persistent fatigue
- chronic pain, especially joint pain
- joint inflammation
- low-grade fever
- rash
- general feeling of being “under the weather”
How are autoimmune diseases diagnosed?
Diagnosis of autoimmune diseases can be difficult since many symptoms are shared by other diseases that do not involve the immune system. Diagnosis begins with a comprehensive physical exam and medical history to look for risk factors and get a clear understanding of symptoms. Lab tests including blood work and urinalysis can help confirm some diagnoses as well as rule out diseases that may cause similar symptoms. It’s also important to realize that while some autoimmune diseases may occur more commonly in families, other diseases are not related to heredity.
How are autoimmune diseases treated?
That depends on the type of autoimmune disease you’re experiencing. Treatment typically is focused on relieving symptoms and working to control or suppress the immune system’s faulty response. Your treatment plan will be customized specifically to your symptoms, your health and your lifestyle.
Osteoporosis
Osteoporosis causes bones to become weak and brittle — so brittle that a fall or even mild stresses such as bending over or coughing can cause a fracture. Osteoporosis-related fractures most commonly occur in the hip, wrist or spine.
Bone is living tissue that is constantly being broken down and replaced. Osteoporosis occurs when the creation of new bone doesn’t keep up with the loss of old bone.
Osteoporosis affects men and women of all races. But white and Asian women — especially older women who are past menopause — are at highest risk. Medications, healthy diet and weight-bearing exercise can help prevent bone loss or strengthen already weak bones.
There typically are no symptoms in the early stages of bone loss. But once your bones have been weakened by osteoporosis, you might have signs and symptoms that include:
- Back pain, caused by a fractured or collapsed vertebra
- Loss of height over time
- A stooped posture
- A bone that breaks much more easily than expected
10 Tips to Ease Osteoarthritis Symptoms on Your Own, at Home.
Make an appointment with our rheumatologist Dr. Henein for your personal diagnostics and to answer any questions you might have.
If you have any comments or questions, please call, email, or use the form below.
All fields are required
Read this privacy note before emailing. Protecting the privacy is extremely important to us and the HIPAA privacy rule mandates it. The privacy rule does not prohibit the use of unencrypted communication, if the patient or the parent of a patient prefers it, requests it or initiates contact with it. Please keep in mind that we cannot guarantee your privacy via the contact form below or via email from your email provider. There is a risk that a third party may be able to obtain information during transmission or while stored on a computer.
Depending on our workload, we will get back to you regarding any question in 2 business days.
(586)226-5555
info@HeneinArthritis.com
39621 Garfield Rd. Clinton TWP, MI 48038

“Dr. Henein is an outstanding, caring and one of the best doctors I have ever seen!! She is very understanding, patient and receptive in regards to listening to me concerns. She takes the time to answer as many questions that I have and never rushes out the door. She literally listens and cares about what you have to say, she has helped me so much that it’s difficult to express in words my gratitude. I can honestly say that Dr. Henein is truly a blessing. The entire staff is also very friendly, helpful and professional. If anyone needs the BEST Rheumatologist in Michigan, you need to contact Dr. Henein.”
CARLOS WINDHOLZ
Patient
10/12/2020